Introduction: Ongoing sickle cell disease (SCD) gene therapy clinical trials in the United States and other high resource countries have shown promising results, and several therapies are under U.S. Food and Drug Administration review in 2023. Despite these advances, the current evidence-based practices are not accessible to much of the world's sickle cell population. As treatment advances are made for SCD, the integration of these therapies in sub-Saharan African countries-which have the highest prevalence of SCD-requires a global partnership. Sierra Leone ranks 9 th in burden in sub-Saharan Africa with annual SCD births between 4000-5000. Efforts are underway in Sierra Leone to improve awareness and healthcare infrastructure for the SCD population; however, the country still lacks a national screening program for diagnosis and faces challenges in providing comprehensive care across the lifespan. This study examines adult SCD patients' knowledge of current evidence-based care and novel gene therapies in Sierra Leone.
Methods: In 2021-2022, a cohort (n=123) of adults living with SCD in Sierra Leone were surveyed as part of the INSIGHTS Study (NCT02156102). A mixed-methods recruitment strategy was used, including via public service announcements hosted on local radio stations, information disseminated via a WhatsApp group, and snowball sampling. Recruitment was conducted in two settings, one urban (Freetown) and one rural (Kono). Participants completed this cross-sectional study from September 2021-February 2022. Questions were asked regarding participants' perspectives and knowledge of hydroxyurea, the current standard of care treatment for SCD, and novel experimental gene therapy.
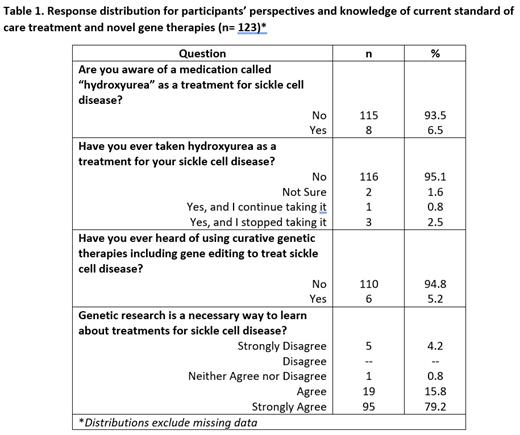
Results: The mean age of respondents was 23.6 years (range 18-63). The majority of respondents were female (65.6%), educated at or above the senior secondary school level (78.7%), and students (70.3%). Respondents predominantly had the HbSS genotype (89.4%). Most study participants lacked awareness of hydroxyurea and gene therapy (93.5% had never heard of hydroxyurea; 95.1% had never taken hydroxyurea; 94.8% had never heard of gene therapy for SCD treatment) (Table 1). Despite this gap in knowledge, the majority (95.0%) agreed that genetic research is a necessary way to learn about treatments for SCD (Table 1).
Discussion: Our results highlight disparities in current standard of care treatment and knowledge in a country with a high prevalence of SCD. While our cohort indicated a favorable attitude toward SCD research and a willingness to participate, these results highlight a significant barrier for successful implementation of current treatment and the adoption of curative genetic therapies in limited resource settings like Sierra Leone. Given the significant lack of knowledge around hydroxyurea, it is important that public health initiatives and research should be directed toward both established standard of care and creating awareness of experimental therapies.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal